A 40 year old male with abdominal pain
July 31,2023
Hi,I am Athram Divya Sri 5th semester student.This is an online elog book to discuss our patient health data after taking his consent.this also reflect my patient centered online learning portfolio.
CASE SHEET
CHIEF COMPLAINTS:
c/o Abdomen pain since 4 days
HOPI:
Patient was apparently asymptomatic 4 days back then developed pain over the left hypochondriac region since 4 days radiating to the right hypochondriac region
C/o vomiting since 4days ,3 episodes watery in consistency ,non-blood stained,non foul smelling
No c/o fever , decreased urine output ,loose stools
H/o Burning micturition since 2 days
C/o SOB , palpitations, orthopnea,pnd
PAST HISTORY:
Not a known case of HTN,DM,Asthma,Epilepsy.
PERSONAL HISTORY:
Diet - Mixed
Appatite - Normal
Sleep - Normal
Bowel and Bladder -Regular.
Allergy - None
Addictions -Alcohol addiction since 10 years last consumption was 4 days back.
FAMILY HISTORY:
No history of similar complaints in the family.
GENERAL EXAMINATION:
The patient is conscious,coherent and cooperative; well oriented to time,place and person.
Pallor - absent
Icterus- absent
Clubbing-absent
Cyanosis-absent
Lymphadenopathy-absent
Edema - absent
VITALS:
Temperature - 98.6 F.
Blood pressure - 140/90 mmHg
Pulse rate - 85/ minute
Respiratory rate - 18/minute
SYSTEMIC EXAMINATION:
CVS:
S1 and S2 heard.
No addded thrills or murmurs heard
RESPIRATORY SYSTEM:
Normal vesicular breath sounds heard.
Bilateral air entry present.
ABDOMEN:
INSPECTION:
shape of abdomen - distended
umbilicus -central
no sinuses
No scars
PALPATION:
Tenderness+ over hypochondriac region
Fluid thrill +
Puddle sign +
PERCUSSION:
No shifting dullness
AUSCULTATION:
Bowel sounds +
CNS:
Conscious and coherent.
Normal sensory and motor responses.
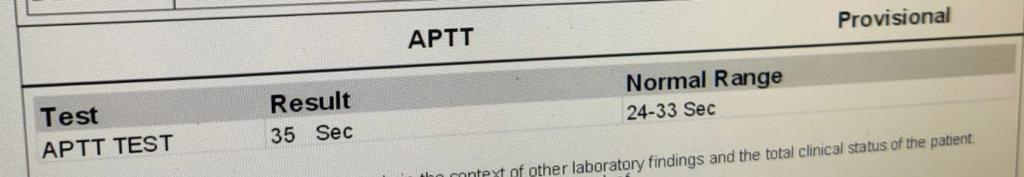
INVESTIGATIONS