A 35 year old female with abdomen pain
September 23,2022
Hi,I am Athram Divya Sri 3 rd semester student.This is an online elog book to discuss our patient health data after taking his consent.this also reflect my patient centered online learning portfolio.
CASE SHEET
CHIEF COMPLAINTS:
A 35 year old female,who is a housewife resident of miryalaguda came to the OPDwith chief complaints of
Pain in the upper abdomen since 4 days
Bilateral loin pain since 4 days
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 5 days back.She developed upper abdominal pain and bilateral loin pain 4 days back for which she was taken to a RMP docter.pain is sudden onset and gradually progressive in nature it is not relieved with medication
and now she came with complaints of abdominal pain and high grade fever associated with chills and rigor.
PAST HISTORY:
No diabetes
No hypertension
No CAD
No asthma
No tuberculosis
No epilepsy
k/c/o undifferentiated CTD,probable SLE
Anti CCP +
PERSONAL HISTORY:
Married
Appetite - lost
Diet - mixed
Bowl movement - regular
Burning Micturition
Sleep- normal
No allergies
FAMILY HISTORY:
Not significant family history
PHYSICAL EXAMINATION:
General examination:
Patient is conscious coherent cooperative
No Pallor
No clubbing
Temperature : Afebrile
Pulse rate : 68/min
Respiratory rate : 16 per minute
Blood pressure : 110/70 mm of Hg
sPO2 : 98%
Systemic Examination
Cardiovascular System
- no thrills
- cardiac sounds S1 and S2 heard
- no cardiac murmurs
Respiratory System
no dyspnea
No wheezing
central trachea
vesicular breath sounds
Abdomen
Scaphoid shaped abdomen
No tenderness
No palpable mass
Non palpable liver and spleen
Bowel sounds -yes
CNS
Patient was conscious
Normal speech
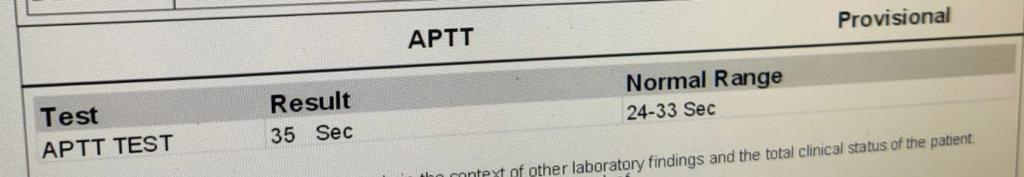
INVESTIGATIONS: